Therapy Techniques Video Library
Watch detailed video demonstrations of our therapy techniques and exercises.
Contact Us
Request an Appointment
For an office evaluation/consultation, please request an appointment.
We accept most major insurances.
Our Goal
Arizona Physical Medicine and Rehabilitation, P.C. is dedicated to providing the most effective, one stop, physician-led team approach to pain management and comprehensive rehabilitation therapy, enabling you to regain functional capacity and improve your quality of life.
We love what we do. Call today to see how Arizona Physical Medicine and Rehabilitation, PC can help you.
Call UsWhy AZPMRPC?
Our newly designed Diagnostic and Treatment Center is the brainchild of Dr. Iqbal Uddin, Board Certified and experienced Physical Medicine and Rehabilitation Physician (Physiatrist) who leads our multi-lingual medical team.
With over 24 years of experience in the medical field, Dr. Uddin is dedicated to ensuring you receive the best quality of care here in the valley.
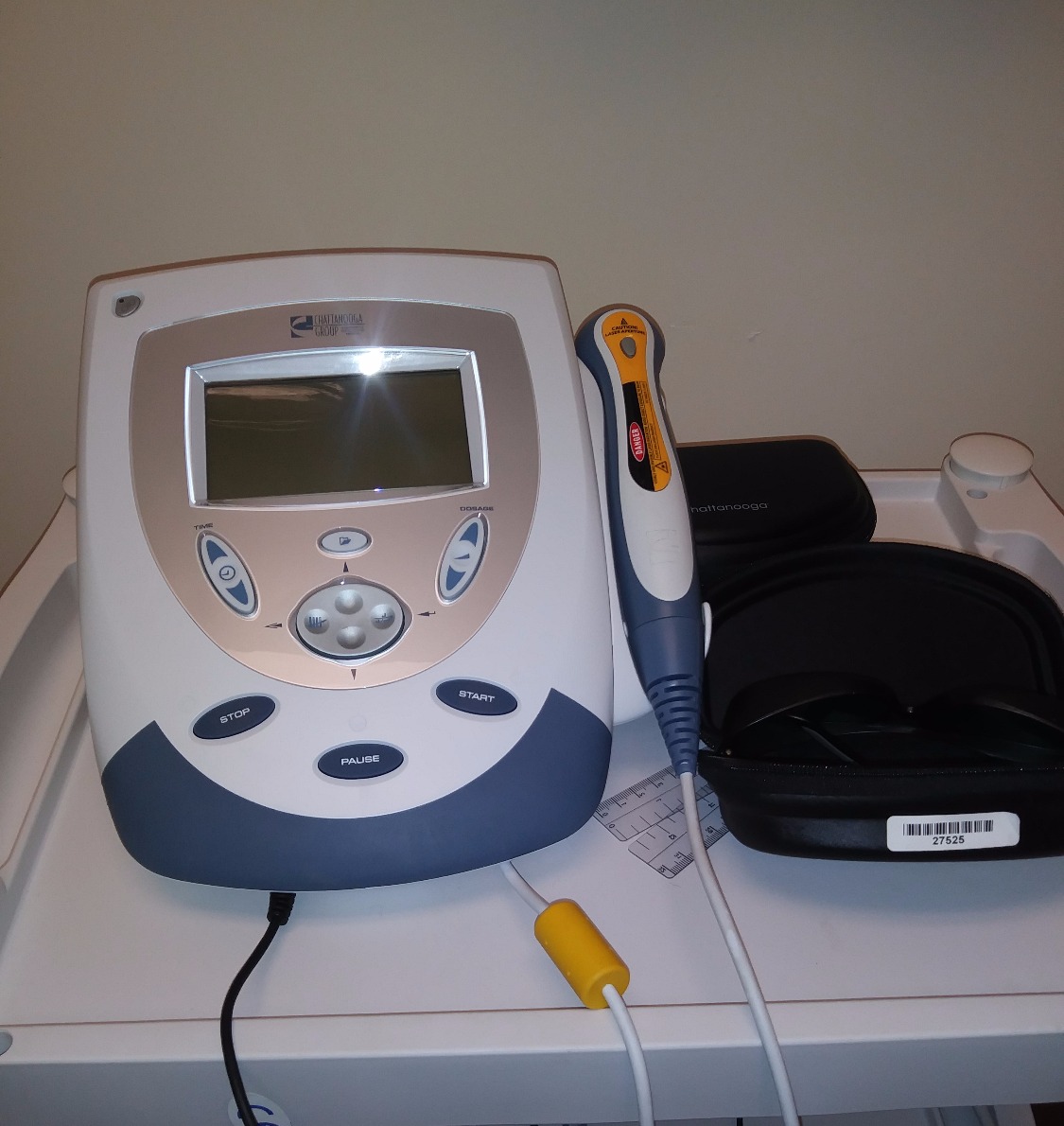
We use state of the art technology and comprehensive physical therapy to design the most effective, multidimensional approach to relieving pain, renewing functional capacity and restoring your quality of life.
We continue to stay informed of the latest innovations in health care and Physical Medicine and Rehabilitation, and work collaboratively with other professionals to coordinate efforts as part of your rehabilitation treatment program.
Read More
What We Treat
We provide expert care for a wide range of conditions.
Neurological Conditions
- Stroke
- Traumatic brain injury
- Spinal cord Injury
- Multiple Sclerosis
- Parkinson's Disease
- Amyotrophic Lateral Sclerosis
- Carpal Tunnel Syndrome
- Neuropathy
Diagnostic
- EMG/Nerve Conduction Study
- Neuropathy
- Radiculopathy
Musculoskeletal Conditions
- Osteoarthritis
- Rheumatoid arthritis
- Fibromyalgia
- Back pain
- Neck pain
- Plantar Fasciitis
- Trigger Finger (Stenosing Tenosynovitis)
Post-operative
- Joint replacement
- Amputation
- Flexor tendon repair
Sports Injuries
- Achilles Tendonitis
- Iliotibial Band Syndrome
- Medial Epicondylitis
- Lateral Epicondylitis
- DeQuervain's Tenosynovitis
- Rotator Cuff Tear/pathology
Pediatric Functional and Developmental Disorders
- Cerebral Palsy
- Muscular Dystrophy
- Spina Bifida
Visit Us
Address:
5690 W Chandler Blvd, Ste 2, Chandler, AZ 85226
Contact:
Email: info@azpmrpc.com
Tel: (480) 878-7425
Fax: (480) 207-1025
Office Hours:
Mon-Fri: 9am to 5pm
Sat & Sun: Closed
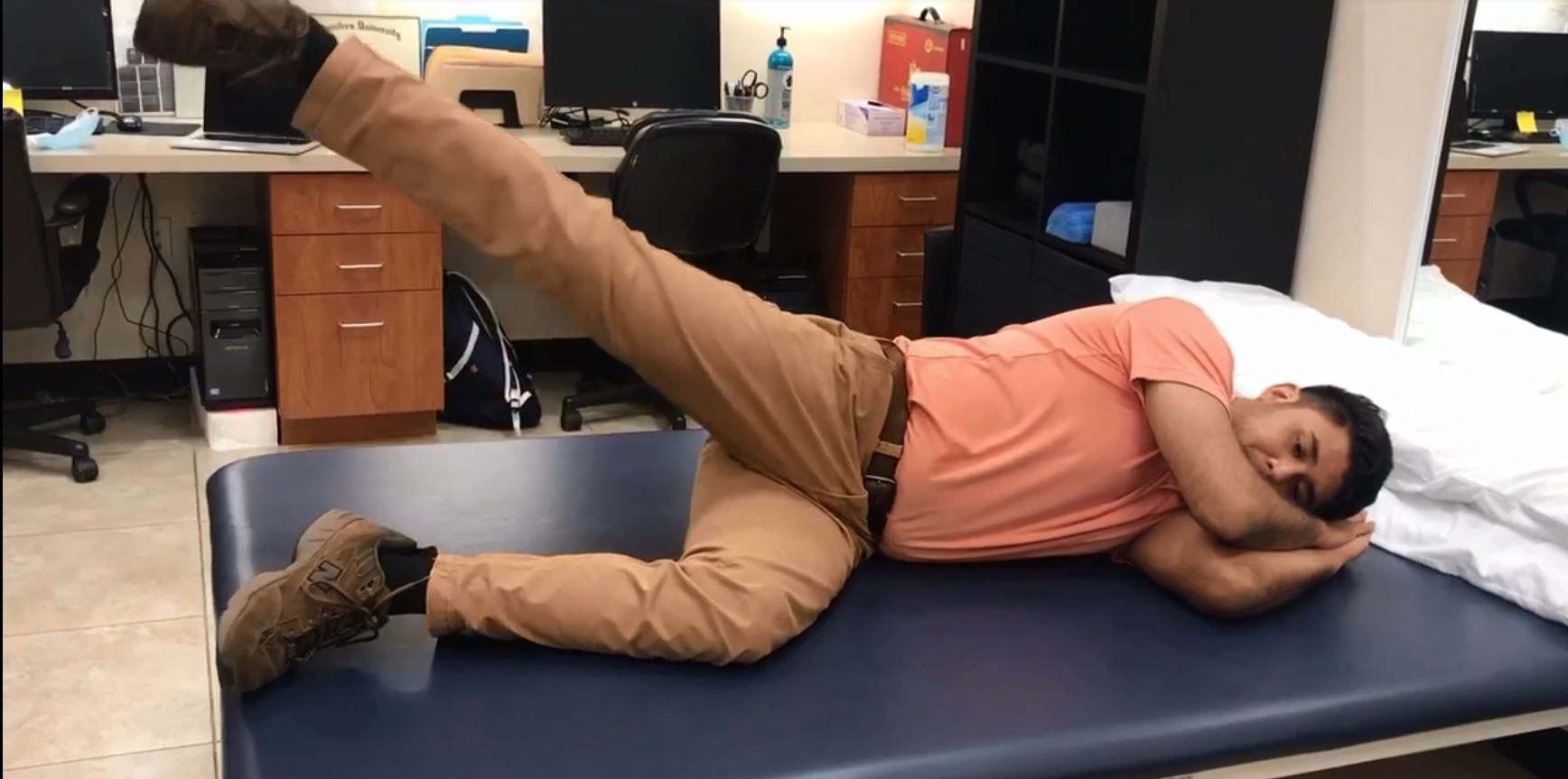
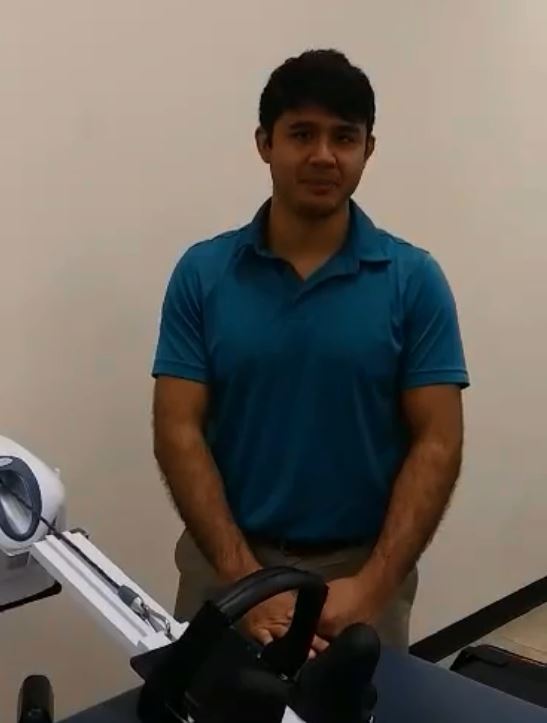
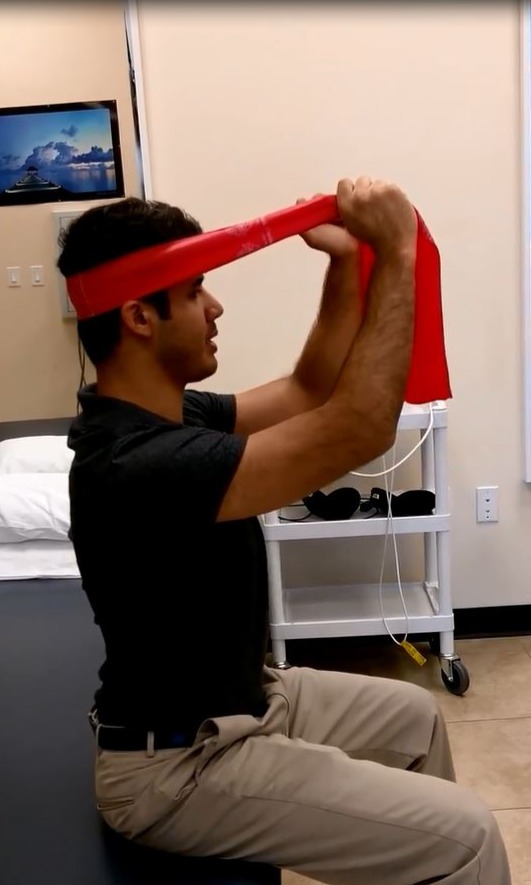
Exercise Therapy Techniques
Targeted exercises designed to restore mobility, strength, and function.
Therapy Modalities
Explore our advanced therapy treatments and equipment